Waiting for the Village; birth
You might be wondering why an economics blog is talking about childbirth, but we can deduce a lot from a society based on the maternal and infant care provided before, during and after the birth of a child.
WAITING FOR THE VILLAGE
Emma Woods
5/18/202410 min read
I want to share some information that I wish I had known before the birth of my first child;
PLEASE EDUCATE YOURSELF ON YOUR RIGHTS DURING PREGNANCY AND CHILDBIRTH. Key rights are listed below, but go to Birthrights, follow birth educators on Instagram such as @BetterbirthUK @NakedDoula @Kemibirthjoyjohnson
You can give birth where you want. Doctors, midwives or anyone else don't have to give you "permission". Medical staff can restrict certain options but it is your right to birth at home if you wish. The only exception to this is if you lack mental capacity; see here for more advice on this.
"In any society the way a woman gives birth and the kind of care given to her and the baby points as sharply as an arrowhead to the key values of the culture" Sheila Kitzinger
You might be wondering why an economics blog is talking about childbirth, but we can deduce a lot from a society based on the maternal and infant care provided before, during and after the birth of a child. I will add a trigger warning to this blog as it mentions maternal death and stillbirth.
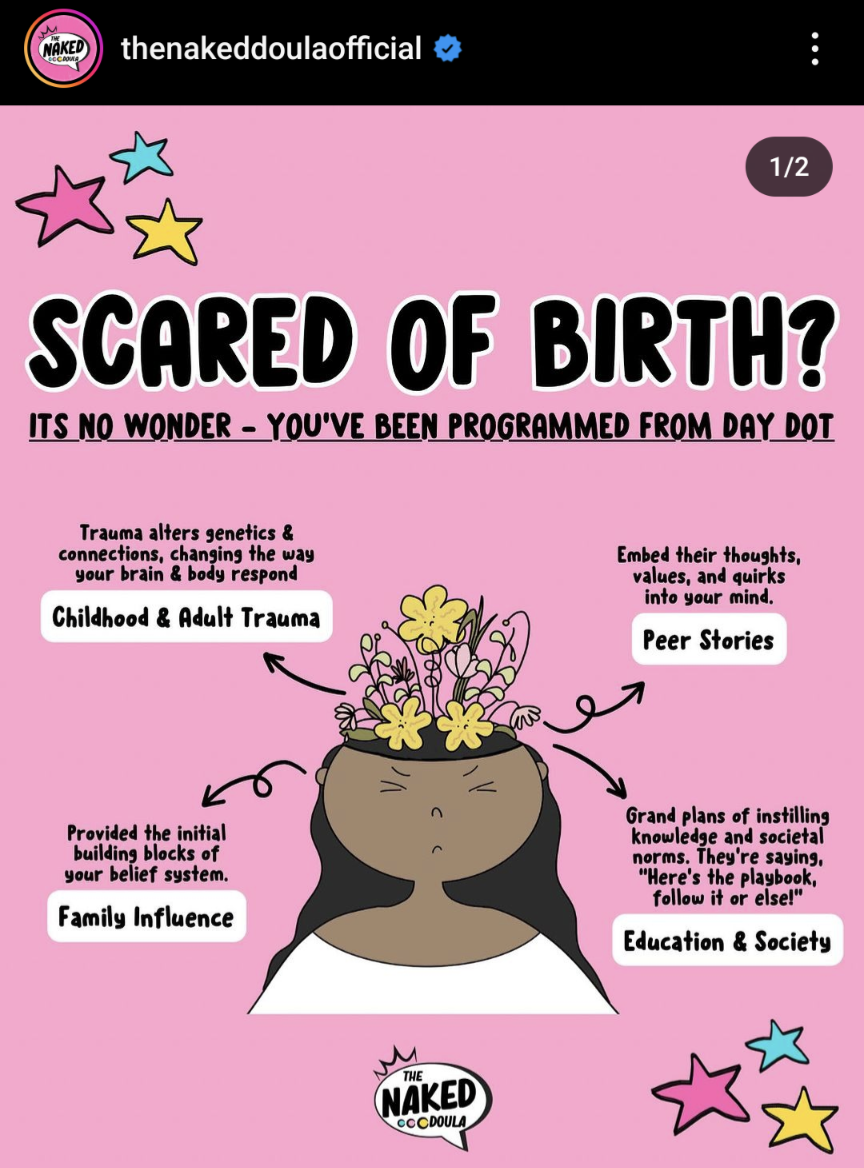
Before diving in I invite you to reflect on the images, stories or ideas you have around birth. Where have these come from? Some of the key narratives I heard when I was pregnant;
Birth is dangerous
Hospital is the safest place to give birth
Homebirth is risky
Doctors know best
I invite you to reflect on these narratives as we explore where they come from and who is perpetuating them. Let's start where the previous blog ended, with men entering birthing rooms, something that shifted the focus away from midwives and wise women and made birth a medical event.
"Birth is a natural event, that occasionally needs medical help, not a medical event that occassionally happens naturally" @Kemibirthjoyjohnson
Barber surgeons started to appear around 400 years ago when Peter Chamberlen invented forceps to "rescue" women and their babies during complicated births. Naturally women were banned from using such instruments and "man midwives" became more common. During industrialisation the women or "gossips" that had previously supported their friends, neighbours and family during labour and birth were no longer available due to their need to work. The traditions of female centered births and knowledge was slowly eroded through the medicalisation of birth and demonisation of wise women and midwives.
We have now come so far from physiological birth that many midwives and even fewer obstetricians have ever witnessed an undisturbed birth.
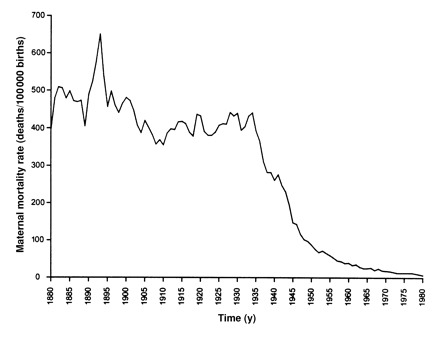
Undoubtedly, there have been great strides in reducing maternal death rates over the last 80 years with the risk of women in England Wales dying 40-50 times lower than 60 years ago, although much of this can be attributed to better santitation, antibiotics and access to healthcare rather than obstetric practice itself.
However comparing data across countries, research finds that "maternal mortality rates were very high in countries, states, regions or areas where most deliveries were performed by physicians, especially in the hospital". This was in part due to sugical interference in birth, with "prophylactic forceps" and the widespread use of choloform used in uncomplicated deliveries between 1870-1940 in Britain. Anyone who's watched the Crown will have seen the Queen's experience of Twilight Sleep where drugs were used to induce a drowsy, amnesic state to relieve the pain of childbirth.
has medicalisation made birth safer?
Of particular note was the incidence of maternal mortality and social class, and not in the direction you might assume. Whereas infant mortality was closely linked to social class with the highest infant mortality linked to the poorest and working classes; the inverse relationship was found with maternal mortality.
In 1930-22, women in the highest social class saw maternal mortality rates of 444 per 100,000 births, compared to 389 per 100,000 births for unskilled labourers. This is believed to be because women in the upper classes were more likely to be treated by physicians and undergo surgical interference, compared to the working class women who were served by midwives.
fast forward to today....
The data tells us that since 2004 maternal death rates in the UK have been trending downwards, as have stillbirth rates since the 1980s. So in some respects birth could be considered safer than ever; however worringly the most recent data from 2020-22 shows the highest maternal UK death rate in 20 years. These statistics also hide the disparities between different groups of women.
Race and deprivation are directly linked to maternal death rates
The risk of maternal death remains almost four times higher for Black women and two times higher for Asian and mixed ethnicity women, than for white women. Women from the most deprived areas have a mortality rate twice as high as women living in the least deprived areas. Black, Asian and mothers from deprived areas are also more likely to experience still birth or neonatal death. Whilst the causes of maternal and infant death are often complex, a recent report by the Women and Equalities Committee found examples of systemic racism which perpetuated racial or ethnic stereotypes. Research by Birthrights found that "Black, Brown and mixed ethnicity women and birthing people often felt unsafe, were ignored and disbelieved, were subject to racism by caregivers, were not given a proper choice or the means to give true informed consent, and were subject to coercion from caregivers, were regularly dehumanised and were disproportionately affected by structural barriers to care."
If you want to dig deeper into how systemic racism is causing maternal death, read this article which is focussed on the US but also applies to the UK context.
IS Hospital the safest place to have a baby?
"A medicalised birth is very likely when you're walking into a medical building packed with medical equipment, ran by medical textbooks, medical staff, medical protocols, medical routine interventions, and surgeons" Flor Cruz
Part One of this series explained how distrust in female bodies to birth our babies has led to increased intervention during pregnancy through testing, scans and medical appointments. With the movement of birth from home and into hospitals we've been led to belive that hospital is the safest place to have a baby but is that the case?
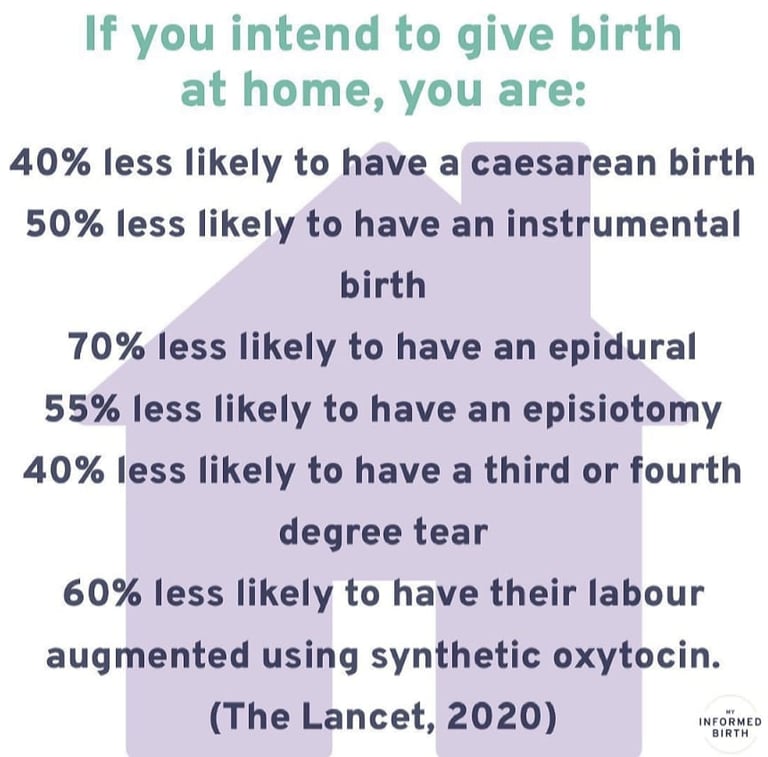
Despite the fear mongering, even just intending to give birth at home reduces your chance of birth interventions and injuries.
Overall only 43% of labours started spontaneously in England in 2022/23, with 57% of births induced or via c-section. Research indicates that children born via spontaneous vaginal birth have fewer short and longer term health problems compared to those born via intervention. Behind these potentially long term impacts to children, lies the potential physical and mental health impacts for birthing parents which is often ignored.
Add to the above the fact that two thirds of maternity units have been deemed "not safe enough" by the Care Quality Commission and it seems bizarre that we are routinely encouraged to birth in a hospital environment.
HOW is all this connected to economics?
Whenever I'm trying to connect the dots between an area of my life and economics I come back to the questions; who benefits? who does it serve? What stories do we tell ourselves and how does the system uphold capitalist tenets of hierarchy, oppression, extraction and exploitation. In the field of pregnancy and childbirth there is also the separation of humans from nature, our instincts and intuition with a movement towards science, evidence and metrics. These ideas are explored in the context of childbirth below;
Doctor knows best
As monitoring and medicalisation of pregnancy increases more and more of us are put under consultant led care. We've been told throughout our lives to put our trust in medical professionals, particularly doctors which still remains a white male dominated profession in the NHS. Western culture places those of higher social class, with greater levels of education towards the top of the hierarchy and we are taught to trust and obey those in such positions of power. Add "good girl" conditioning, the vulnerability and anxiety of pregnancy and we often fall prey to white coat syndrome where we start to agree with their advice even if it goes against our instincts.
Yet, obstetrics as a profession cannot claim to be evidence based when a review of guidelines set out by the Royal College of Obstetricians and Gynaecologists found that only 9% of guidelines published since 2007 were based on level A evidence. 40% weren't evidence based at all and simply driven by "best practice". Something I found shocking was how even medical professions were so swept up in the guidelines and perceived wisdom, that many didn't appear to be able to back up their claims when asked for proof of evidence; so infrequently had anyone dared to question the system.
Something I had never heard of until after my own traumatic birth was Iatrogenesis - the causation of a disease, a harmful complication, or other ill effect by any medical activity, including diagnosis, intervention, error, or negligence. Whilst pregnant people are often told about the risks from their bodies, we are not told about the risks from medical intervention. More on this below.
Control of women's bodies, impatience and inability to wait
Our bodies can no longer be trusted to begin labour at the right time, instead with the medicalisation of pregnancy, test and scans prescribe when labour must begin. Talk of induction begins at 38 weeks in some trusts or earlier based on "risk factors" (see below) and we are pressured to "get things going" with a "harmless" sweep. This further serves to undermine female bodies and their babies to trust their instincts and wait until the baby begins the process of labour.
Assessment of risks
Risk assessment has always been a key part of human life, but we know humans are notoriously poor at actually understanding comparative risk. As Kahneman explained; in the case of loss aversion people go to absurd lengths to avoid risks that are actually negligible.
For women aged over 35 their pregnancy is classed as "geriatric" as the risk of stillbirth increases with age and induction is often recommended to mitigate this risk. When you actually look at the data behind the claim;
According to Havaaldsen et al 2010 the risk of stillbirth at 40 weeks was;
0.84 per 1000 or 0.08% for women aged 20
1.91 per 1000 or 0.19% for women aged 35
1.61 per 1000 or 0.16% for women aged 40
Less than half of birth onsets in the UK are now spontaneous, with a third of births begun through induction. This pressure to birth on a timescale, an inability to wait until your body and the baby is ready is driven by capitalist ideals around time, efficiency and productivity. Often we are told that our baby needs to be induced for medical reasons, however its striking how inductions and caesarians avoid weekends and public holidays. If you want to dive deeper into how western medicine controls labour listen to this podcast.
We know from behavioural economics that how data is presented matters. If the midwife or doctor presented the data as 99.84% of births at 40 weeks to mothers aged over 40 were live births, no doubt that would change the attitude and approach to induction.
Aside from the presentation of risk of inaction, you are very rarely informed of the risk from the intervention. We know that induction increases the likelihood of further intervention and adverse outcomes through the cascade of intervention; 51% of deliveries in 2022/23 were either assisted with instruments or caesaria, but this is rarely talked about.
Finally, in terms of risk assessment questions needs to be asked about the NHS's approach to likelihood and impact of risk particularly in relation to the longevity of impact. If you birth in hospital you are often discharged within days unless there are serious complications. Midwives discharge you from their service within 10-14 days once your baby has returned to birth weight. After that you're on your own. From my experience and looking at the increased incidence of certain types of medical intervention it appears the NHS is risk averse, prefering to intervene to prevent catastrophic loss whilst failing to measure the impacts of interventions that go beyond their immediate care remit. Part three will cover post partum health, but pelvic floor issues, postpartum depression and birth trauma are increasingly common long term side effects of the highly medicalised UK birth system.
Baumol's cost disease
Over time economists expect productivity to increase due to economies of scale, innovation and automation which has been seen in manufacturing but is more challenging in service sectors such as healthcare. This is because low productivity may be a feature of the service being provided; if I go to see my doctor I don't want them to shorten their appointments from 15 minutes to 5 minutes just so they can squeeze more patients in and "increase productivity". In many areas we value this low productivity and pay a premium for it; private schools for example that have smaller class sizes. Baumol recognised that as labour intensive services are less likely to see productivity gains, over time the proportion of national income spent on these labour intensive services would increase. Whilst politicians might lament the increasing cost of public healthcare and some decry the laziness of NHS workers, it is Baumol's cost disease in action, whichis supported by historical data.
Why does this matter? Because whilst politicians refuse to acknowledge this phenomenon, the rising costs of key labour intensive services (which are often publicly funded) such as education and healthcare will continue to be underfunded.
In closing....
You have the right to decline interventions even if it's hospital policy.
If you feel you can't say no, it's not consent. For consent to be valid it must be given voluntarily.
Trust your body and your instincts .
Watch real birth videos and seek out positive birth stories. @Badassmotherbirther has hundreds of beautiful videos that show the immense power and beauty of birth.
Despite the doom and gloom of this blog; after my own first traumatic birth I went on to hire a doula, educate myself on physiological birth and had a beautiful homebirth (against medical advice) that completely changed my view on birth. From my first traumatic birth, to feeling like birthing was a privilege. Birth does not have to be traumatic.
If this blog has brought up difficult feelings please reach out for support. The Birth Trauma Association can offer support and my inbox is always open; emma@flourisheconomics.com. Sending love and solidarity. Emma x
